The Shoulder Joint
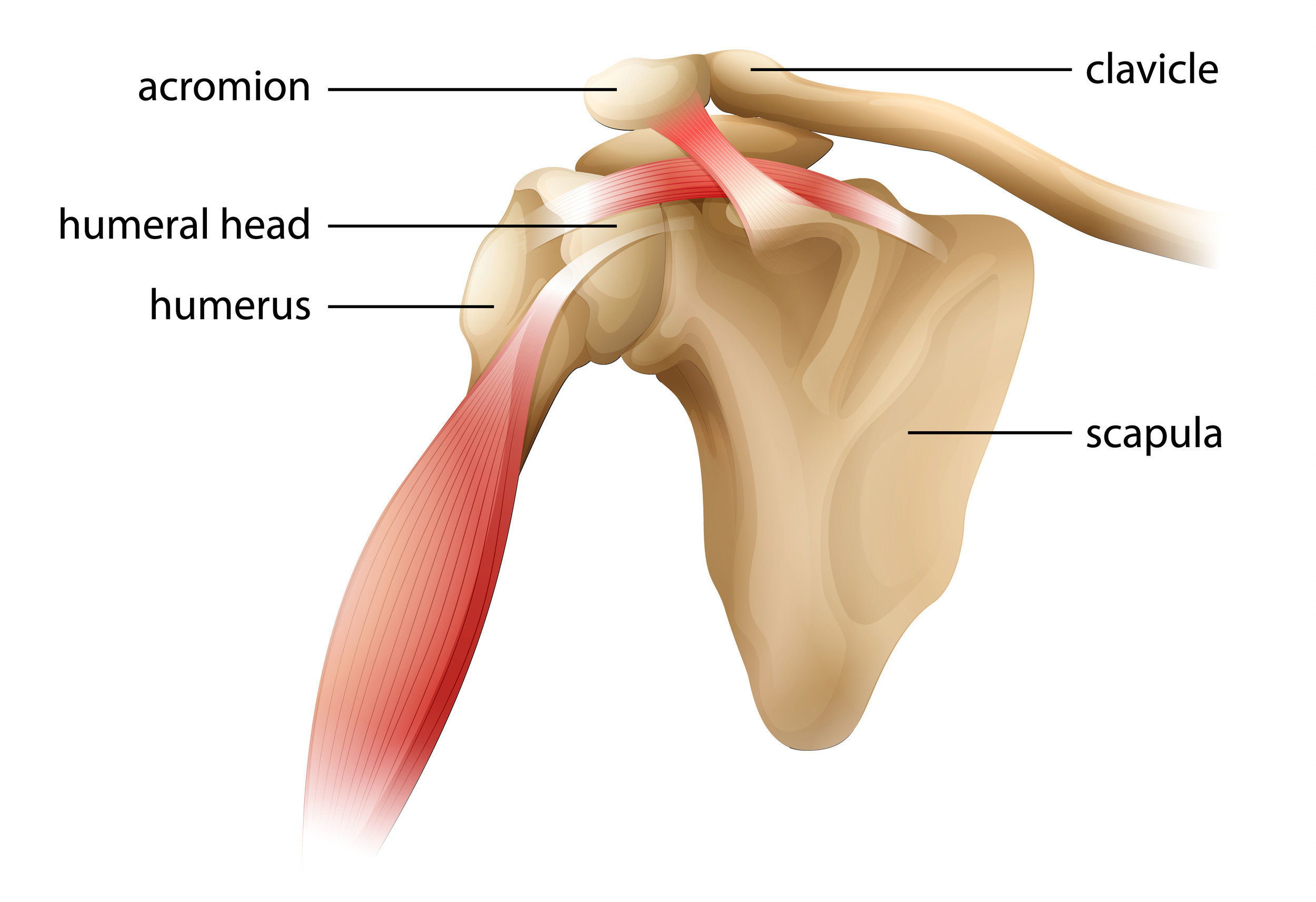
The shoulder joint is arguably the most sophisticated joint in the body, combining a whole hemisphere of movement with the power to throw a javelin. It has a three level design to allow this to happen. Firstly, the scapula (shoulder blade) acts as a mobile platform that is moved by five deep muscles. The clavicle (collar bone) splints the shoulder out to the side. Next, the four small rotator cuff muscles hold the “ball” of the humeral head in the shallow “socket” of the glenoid fossa of the scapula. This joint is cushioned by an oval cartilage “washer” called the labrum. Finally, the power muscles attach over the top of the shoulder joint (eg pec major, lat dorsi, deltoid). All three levels of muscles need to work in balance with each other for the shoulder to function well.
Rotator Cuff Disease
The rotator cuff is comprised of four small muscles that anchor on the scapula and attach around the margin of the humeral head. They are the supraspinatus, infraspinatus, subscapularis and teres minor muscles. When the shoulder is moving, these muscles continually adjust their tension with each other to hold the ball in the joint socket. Because they are relatively small muscles, they are prone to overload and injury. For instance, the supraspinatus muscle can get overloaded and sore from carrying heavy loads (eg suitcases). The tendons of the rotator cuff muscles are increasingly likely to develop tears as we age, with up to 50% of 50 year olds being reported as having a tear on ultrasound. These tears may be a source of pain that comes and goes. Surgery for partial tears has been shown not to be any better than physical therapy at 5 year followup. Glucose prolotherapy or PRP-injections can help heal partial tears and give long term improvement.
Subacromial Bursitis
A bursa is a small fluid-filled sack adjacent to a joint. It normally contains a tiny amount of oily synovial fluid that is designed to reduce friction where a tendon runs over bone. If there is increased friction, the body responds by increasing the amount of fluid in the bursa. The bursal enlargement is called bursitis, but it is generally better thought of as the symptom rather than the root cause of the problem.
One of the limitations of the design of the shoulder joint is that the supraspinatus tendon has to run through the small gap under the acromium of the scapula bone. If there is extra tension through the tendon, the subacromial bursa can enlarge and take up valuable space. This can result in the tendon rubbing under the acromium, causing pain each time the arm is lifted through the horizontal out to the side (painful arc). This is called subacromial bursitis and it can be significantly helped by injecting a steroid solution to shrink the bursa and break the vicious circle. However, the problem frequently returns unless the initial muscle imbalance that led to the bursal enlargement is addressed. A comprehensive musculoskeletal medicine approach addresses both aspects of the problem with both the bursal injection and separate muscular treatments.
Frozen Shoulder (adhesive capsulitis)
Frozen shoulder is a nasty cause of shoulder pain that is most common in peri-menopausal women and diabetics. It’s cause is not well understood but it may be driven by nerve inflammation. Frozen shoulder often starts with a relatively minor shoulder injury or sometimes after surgery. It has three distinct stages:
- Initial hot phase (6-9months) - where the shoulder becomes increasingly painful to movement. Severe shooting pains can be set off with minimal movement and shoulder pain will often disturb sleep. The patient gradually learns to avoid pain by not moving the shoulder. It often becomes hard for patients to comb their hair or reach behind their backs.
- Cold / frozen phase (4-12months) – where the shoulder mercifully becomes less painful but at the cost of markedly reduced movement. Fine adhesions form inside the joint, between the head of the humerus and the surrounding joint capsule (adhesive capsulitis). The shoulder “freezes” up.
- Thawing phase (1-2 years) – where shoulder movement gradually returns but often not completely.
Treatment of frozen shoulder is challenging and works best when the patient presents early. Multiple studies have shown that physical therapy does not improve the clinical course of frozen shoulder. Injection therapies seem to get the best results. Steroid injections into the joint can be helpful to damp down some of the joint inflammation. Local anaesthetic and steroid injections around the major nerve of the shoulder can also be helpful (suprascapular nerve block). Other soft tissue injections appear to be helpful in reducing the amount of muscle pain around the joint. Radiologists are sometimes asked to inject fluid into the joint under pressure to distend the capsule and break down the adhesions (joint hydrodistension). This seems to work in about 30% of cases. Rarely, an orthopaedic surgeon will do the same thing by manipulating the shoulder joint under general anaesthetic, although this is not a gentle procedure.
Acromio-clavicular Joint Injuries
The “A-C” joint is a fibrous joint between the outside end of the collar bone and the acromium of the scapula. It is prone to injury with overhead lifting or direct trauma (eg rugby tackles). Complete A-C joint separation (rare) is best dealt with through urgent surgery. However, partial strains or osteoarthritis can be effectively treated with regenerative injections (either prolotherapy or platelet-rich plasma).
Dr. Chris Homan
MBBS FRACGP FACRRM DRANZCOG PGDipMSM(Otago)