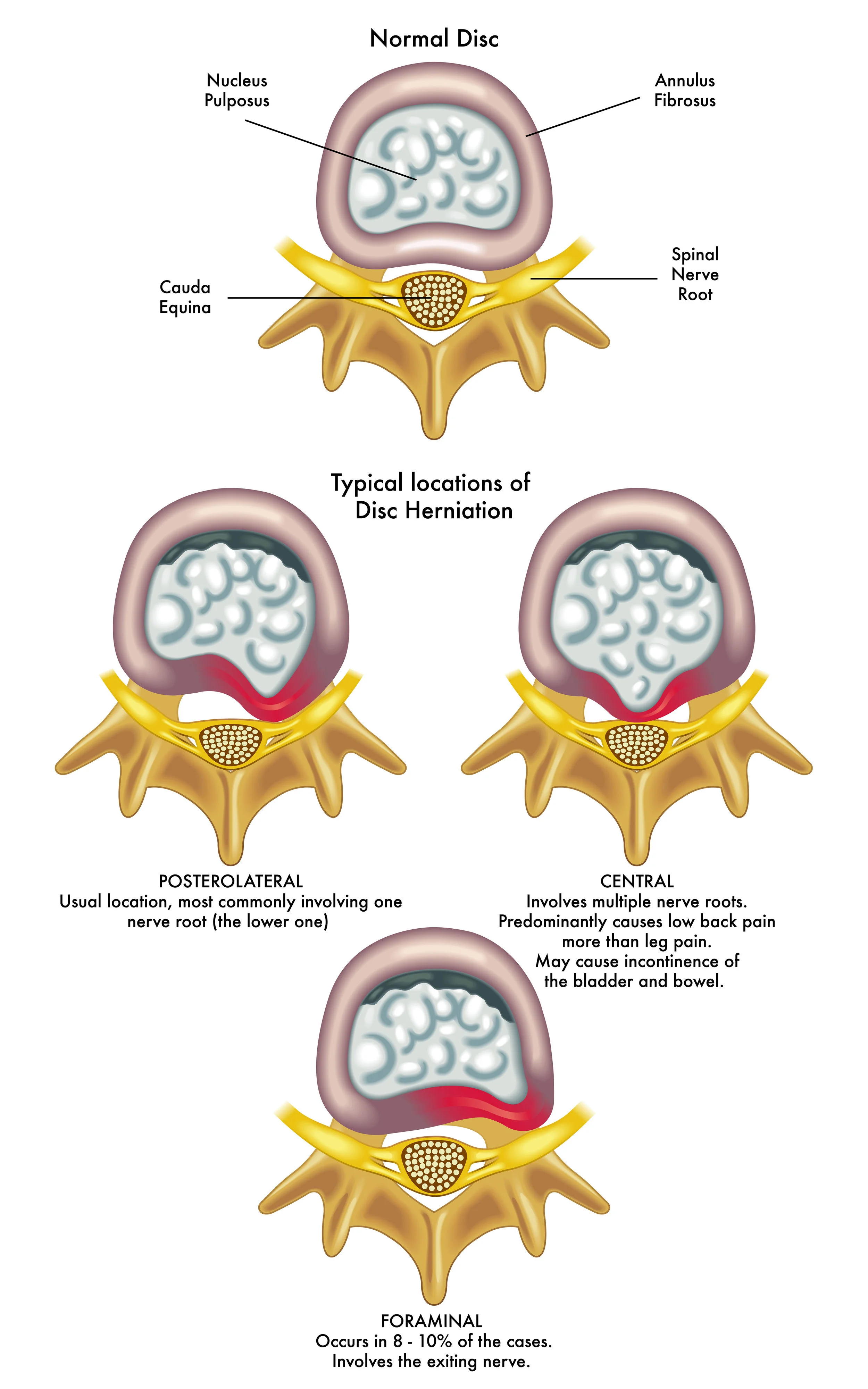
“Intervertebral” discs are the rubbery, shock-absorbing pads between each two vertebral bones in the spine. Each disc has a tough outer cover, called the annulus fibrosis, and a softer gel centre, called the nucleus pulposis. The outer annulus has multiple layers arranged with an alternating fiber orientation for increased strength (like a steel belt radial tyre). The annulus helps prevent excessive movement between vertebrae whilst containing the shock-absorbing gel of the nucleus. A disc prolapse occurs when a weakness in the outer annulus allows the inner gel to protrude out (see arrow in diagrams). It may be described as a protrusion if small, an extrusion if large or as a sequestered segment if it has completely detached.
Disc prolapses are thought to occur because of weakening of the outer annulus, sometimes in combination with an acute mechanical event. They can occur at any age but are most common between the ages of 30 and 50. Risk factors include genetic susceptibility (50% of the risk), being male, heavy lifting or twisting and cigarette smoking. Studies show that 20-35% of adults will have a disc prolapse visible on MRI at any point in time, with most of those people not having any back or leg pain. The prolapsed material tends to resorb over time and the annular tear does have the ability to heal over.
95% of lumbar disc prolapses occur in the last two segments (between the L4-5 or L5-S1 vertebrae). Patients with a disc prolapse may have a history of recurrent low back pain related to progressive weakening of the annulus. Disc prolapses usually only cause major symptoms when they prolapse out to the side – towards where the nerve roots leave the spine. Whilst the pressure of the prolapsed material on the nerve root may cause some numbness or weakness, it is the chemical irritation caused by the gel that irritates the nerve root and causes the pain down the leg. This shooting pain down the leg is often called sciatica.
The good news is that in 70% of cases, sciatic leg pain from disc prolapse settles by itself over 3-6 months. The average outcome 1-2 years after a disc prolapse is similar regardless of what treatment you have. The reason to consider treatment is to try and reduce / shorten pain symptoms, and in rare cases, protect nerve function. An MRI scan is the best way to see what is happening and is performed if there is doubt about the diagnosis or intervention is being considered.
Treatment options for disc prolapse with pain referring to the lower limb:
- Do nothing and allow nature to take its course
- Simple pain relieving tablets (paracetamol, anti-inflammatories)
- Stronger pain tablets (narcotics)
E.g. Targin is a moderately strong pain reliever that lasts for 12 hours and has a second ingredient to lessen constipation. - Physical therapy
A significant amount of the pain associated with disc prolapse and nerve irritation is due to secondary muscle spasm and joint malalignment. Physical treatments that help treat the soft tissues and reduce muscle spasm can be quite helpful in reducing the associated pain. These include various musculoskeletal techniques, including muscular trigger point injections. - Inversion therapy
Gentle traction on the low back can be helpful in reducing the symptoms of disc prolapse. This can be performed by placing a pillow on a kitchen chair and lying across it so that your legs are hanging straight down, gently pulling the low back. Alternately, an “inversion table” can be purchased on the internet and used for 5 minutes, twice a day. Patients should always have someone supervising them when using the inversion table and not have any medical conditions that would make it dangerous. - Pain modifying tablets
E.g. Lyrica is from the anti-epilepsy group of medications and helps to reduce pain signal transmission. It is generally good for a halving of severe nerve pain and is commonly taken for a few months whilst the worst of the pain settles. “Getting to know you” side effects are common when starting Lyrica and these tend to be avoided by building the dose slowly over one week. - Oral steroid medication
Prednisone steroid tablets can help pain by reducing early inflammation and swelling. It should only be taken for 7-10 days because side-effects rapidly increase after that. - Steroid nerve root sleeve block
CT-guided injection precisely delivers a steroid solution around the prolapse to damp down the inflammation of the nerve root. This minimally invasive intervention has been shown to settle symptoms in more than 50% of cases. - Surgery
In rare circumstances, spinal surgery is indicated to relieve severe leg pain or release pressure on nerves. Microdiscectomy is the most common operation and involves removing the prolapsed nuclear material with minimal disruption to the surrounding tissues. Unfortunately any surgery carries risk of complications and modern spinal
surgeons tend to do an excellent job of informing patients about these.
An extremely rare condition is Cauda Equina Syndrome, where a very large disc prolapse compresses the nerves in the spinal canal. The symptoms include numbness in the groin and inner thighs, loss of control over bladder and bowels and leg weakness. Anyone who thinks they may have this condition should immediately present to a hospital emergency department for assessment.
Dr. Chris Homan
MBBS FRACGP FACRRM DRANZCOG PGDipMSM(Otago)
Principal reference: The Biomechanics of Back Pain 3rd Ed (2013) Adams M., Bogduk N., Burton K., Dolan P. (Churchill Livingstone)