The pectoralis major muscle (see below) appears to be the dominant mechanical influence on upper body pain. This strong muscle on the front of our chest tends to adaptively shorten with our modern habitual flexed postures (computer / smart phone / driving). Once our shoulders and head flex forward, the problem is compounded by the action of gravity. This favours overload pain in a series of mainly neck and shoulder muscles, whose pain referral patterns have been known since Professor Kellgren’s experiments on British medical students in the 1930’s!
Pectoralis major muscle
Once our shoulders and head flex forward, the problem is compounded by the action of gravity
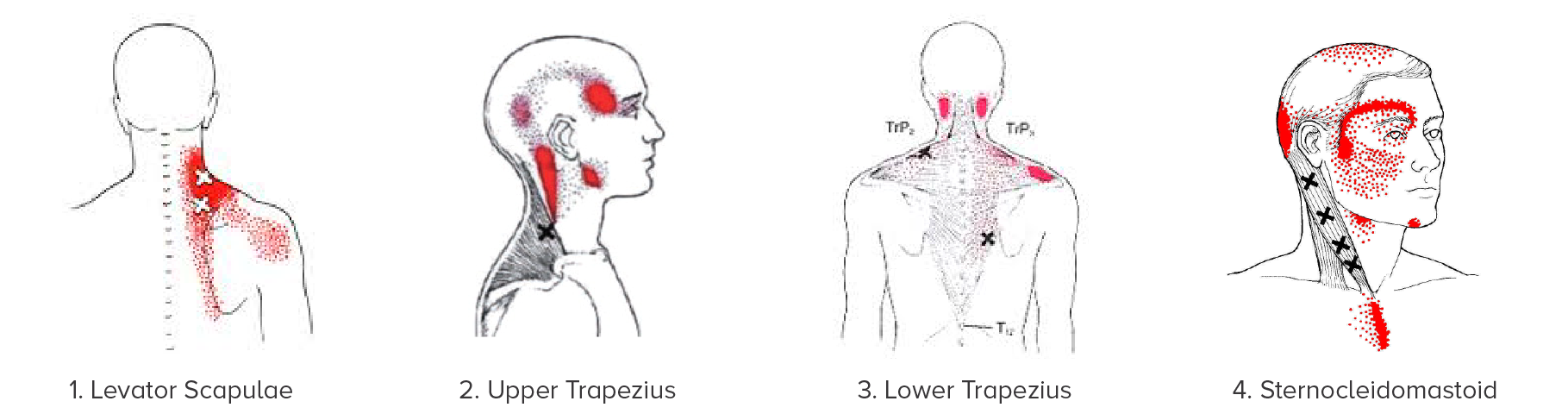
Common “victim” muscles that are overloaded by pectoral muscle shortening include (see diagrams below):
- Levator scapulae » neck base / yoke pain that can run inside the shoulder blade.
- Upper trapezius » side-of-head “tension” headache
- Lower trapezius » base-of-skull headache
- Sternocleidomastoid » forehead and behind-the-eye pain (migraine-like)
Treat the cause of neck pain and headaches.
The vast majority of physical therapy seems to target the overloaded, painful tissues. Whilst this can provide transient symptom relief, it is highly unlikely to lead to lasting improvement for chronic pain. Definitive treatment of upper body muscular overload pain usually involves lengthening the pectoral muscles. The most powerful way to do this is with muscular trigger point injections, which elicit a spinal reflex to help reset the muscle length. 1-2 minutes of needling will frequently bring about as much change as 1-2 months of stretching! Unfortunately breast implants prevent needling the pectoral region and other techniques have to be used. Patients with chronic upper body pain are likely to benefit from improved desk/driving/standing postures and should perform simple pectoral muscle stretches daily.
Migraines
Migraines are a particular kind of headache that can be exceptionally debilitating. They are characterized by throbbing pain in one side of the head that typically lasts 4-72 hours. Migraines are frequently associated with nausea (80%) and vomiting (50%), with one-quarter being preceded by visual changes (auras). They tend to occur in genetically-susceptible individuals (70% have a close family history of migraine) and are more common in women (75%). The “neurovascular” theory of migraine holds that the release of inflammatory chemical messengers (eg substance P, CGRP) from hyper-irritable nerves leads to a cascade of pain and associated symptoms.
Migraines can be precipitated by various triggers:
- Food e.g. chocolate, cheese, caffeine, alcohol, additives (incl MSG, aspartame)
- Sensory stimulation eg bright or flickering lights, loud sounds, strong odours
- Stress, sleep deprivation, hormonal changes
Migraine management includes:
- Avoidance of triggers
- Acute drug treatments – drugs taken early in a migraine attack
- Includes aspirin, triptans (e.g. Maxalt, Relpax) - Preventative drugs – taken daily to reduce migraine attacks
- Includes beta-blockers, anti-inflammatories, anti-epileptics
- Each medication only has about a 30% chance of improving an individual’s migraines and typically has to be trialed for 3-6 months to assess its effectiveness - Botox injections are available from neurologists for patients with chronic migraine pain for >15 days per month. These temporarily paralyse scalp muscle spasm that might lead to migraine. Interestingly, the original botox studies show that most of the same improvement occurs if saline is injected rather than botox.
- Electrotherapy – Cefaly is a new device which is designed to reduce migraines
"Musculoskeletal Migraines"
Many migraine sufferers also experience neck pain and headache. Typically they will be aware that if their neck pain and headache worsens, then they are at greater risk of it snowballing into a migraine. These are the patients who can benefit greatly from musculoskeletal treatment to address the cause of their underlying neck pain and headache. My experience is that these patients can have dramatic reductions in the frequency and severity of their migraines once their neck pain and headaches are addressed. Presumably this reduces the pain signals into the brain and keeps them below a threshold that would trigger a migraine in susceptible individuals.
Dr. Chris Homan
MBBS FRACGP FACRRM DRANZCOG PGDipMSM(Otago)